If you’ve ever reached for a dietary supplement to boost your health, you might be unknowingly increasing your risk of serious liver damage—and potentially liver cancer. Recent research reveals a disturbing connection between certain dietary supplements and liver cancer development, with herbal and dietary supplements now accounting for approximately 20% of all drug-induced liver injury cases in the United States. This represents a dramatic increase from just 7% in 2004-2005, signaling a growing public health crisis. The liver serves as your body’s primary metabolic processing center, making it uniquely vulnerable to the hidden toxins in supplements that operate under minimal regulatory oversight.
Unlike prescription medications that undergo rigorous safety testing before reaching consumers, dietary supplements enter the market with no requirement to prove they’re safe or effective. This regulatory gap has enabled more than 80,000 different supplements to flood the U.S. market—a twentyfold increase since 1994. While most supplement users expect health benefits, emerging evidence shows certain products cause severe liver injury patterns that may increase long-term cancer risk. Understanding which supplements are linked to liver cancer could literally save your life, as the damage often occurs silently before symptoms appear.
This article exposes the specific dietary supplement linked to liver cancer risks you need to avoid, reveals which products triggered Hawaii’s deadly liver injury outbreak, and provides actionable steps to protect your liver while still getting the nutrients you need. You’ll learn why vitamin E actually reduces liver cancer risk by 40%, how to spot dangerous ingredients on labels, and what to do if you suspect supplement-related liver damage.
Why 20% of U.S. Liver Injuries Now Come from Dietary Supplements
The alarming rise in supplement-related liver damage represents one of modern medicine’s most under-recognized public health threats. Data from the Drug Induced Liver Injury Network (DILIN) shows herbal and dietary supplements now cause approximately 20% of all hepatotoxicity cases in America—a staggering increase from just 7% fifteen years ago. This surge directly correlates with the explosive growth in supplement sales, which skyrocketed from $9.6 billion in 1994 to $36.7 billion in 2014 as consumers increasingly turned to these products for weight loss, muscle building, and general wellness.
What makes supplements uniquely dangerous to your liver? Unlike pharmaceutical drugs that undergo mandatory pre-market safety testing, supplements operate under the Dietary Supplement Health and Education Act of 1994, which classifies them as foods rather than drugs. This regulatory loophole means manufacturers can sell products without proving safety or efficacy, placing the burden on the FDA to demonstrate harm after damage has already occurred. The liver processes everything you ingest, making it the first organ to encounter potentially toxic compounds in supplements—often at concentrations far exceeding what occurs naturally in foods.
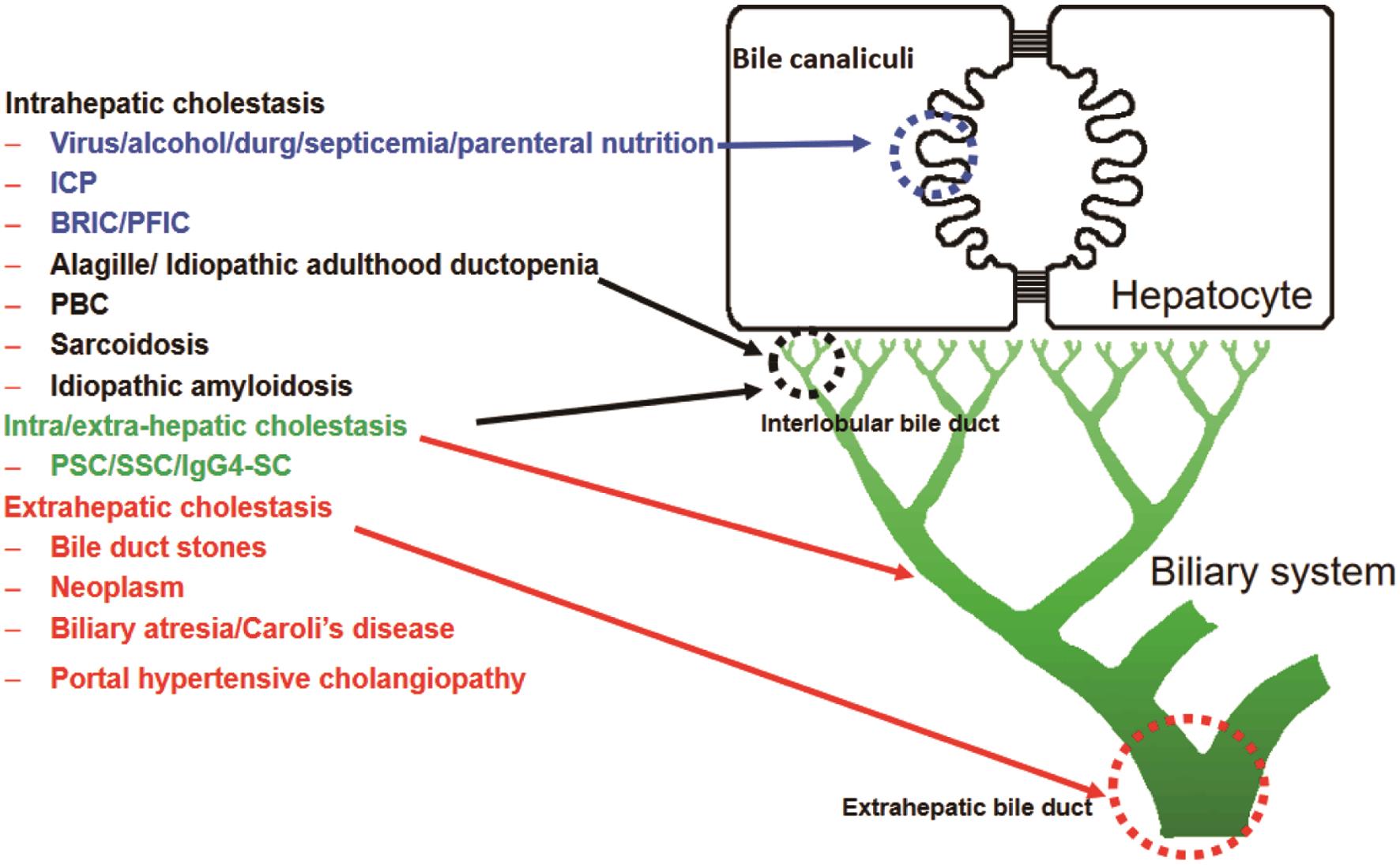
How Supplement Liver Damage Differs from Prescription Drug Injury
Supplement-induced liver injury presents in distinct patterns that healthcare providers are increasingly recognizing:
- Cholestatic injury: Characterized by severe jaundice with bilirubin levels reaching 40-50 mg/dL while liver enzymes remain only mildly elevated (1-3x normal). This pattern is typical with anabolic steroid supplements.
- Hepatocellular injury: Resembles viral hepatitis with dramatically elevated ALT/AST levels (often 10-20x normal), dark urine, and jaundice. Common with green tea extract and multi-ingredient products.
- Mixed injury: Combines elements of both patterns, frequently seen with complex supplement formulations.
Pro Tip: If you’re taking supplements and notice unexplained fatigue, yellowing of the eyes, dark urine, or abdominal pain, stop the supplement immediately and get liver function tests—even if you’ve taken it for months without issues. Some supplement injuries develop after prolonged use.
Anabolic Steroids: How Bodybuilding Supplements Cause Severe Cholestatic Jaundice
Bodybuilders and fitness enthusiasts seeking muscle gains often turn to anabolic steroid supplements without realizing their devastating impact on liver health. These products trigger a distinctive pattern of liver injury characterized by intense jaundice with hyperbilirubinemia reaching levels of 40 to 50 mg/dL—ten times the normal upper limit—while serum aminotransferases remain only modestly elevated (1-3x normal). This “bland cholestasis” pattern shows minimal inflammation on liver biopsy but causes prolonged jaundice lasting 2-4 months.
Why Anabolic Steroid Liver Damage Is Particularly Dangerous
The mechanism behind this injury involves selective canalicular dysfunction without significant hepatocyte necrosis, suggesting impairment of bilirubin and bile acid secretion. While death from liver failure is uncommon, severe cases can trigger renal dysfunction requiring temporary dialysis. More concerning for long-term health, case reports link chronic anabolic steroid use to benign liver tumors including peliosis hepatis and hepatic adenomas—conditions that may potentially transform into liver cancer with prolonged exposure.
Critical Warning: Supplements marketed as “prohormones” or “testosterone boosters” often contain actual anabolic steroids despite labeling claims. These products cause the most severe and prolonged cholestatic injury patterns among all supplement categories.
Green Tea Extract Dangers: 50+ Liver Injury Cases and 10% Fatality Rate
Green tea extract supplements, frequently marketed for weight loss and antioxidant benefits, have been linked to more than 50 documented cases of clinically apparent acute liver injury with jaundice since 2006. The typical presentation involves an acute hepatitis-like illness developing within 1-3 months of starting the product, with symptoms including fatigue, loss of appetite, dark urine, and jaundice. Laboratory findings show marked elevations in serum aminotransferases with a hepatocellular pattern of injury.
What Makes Green Tea Extract Hepatotoxic
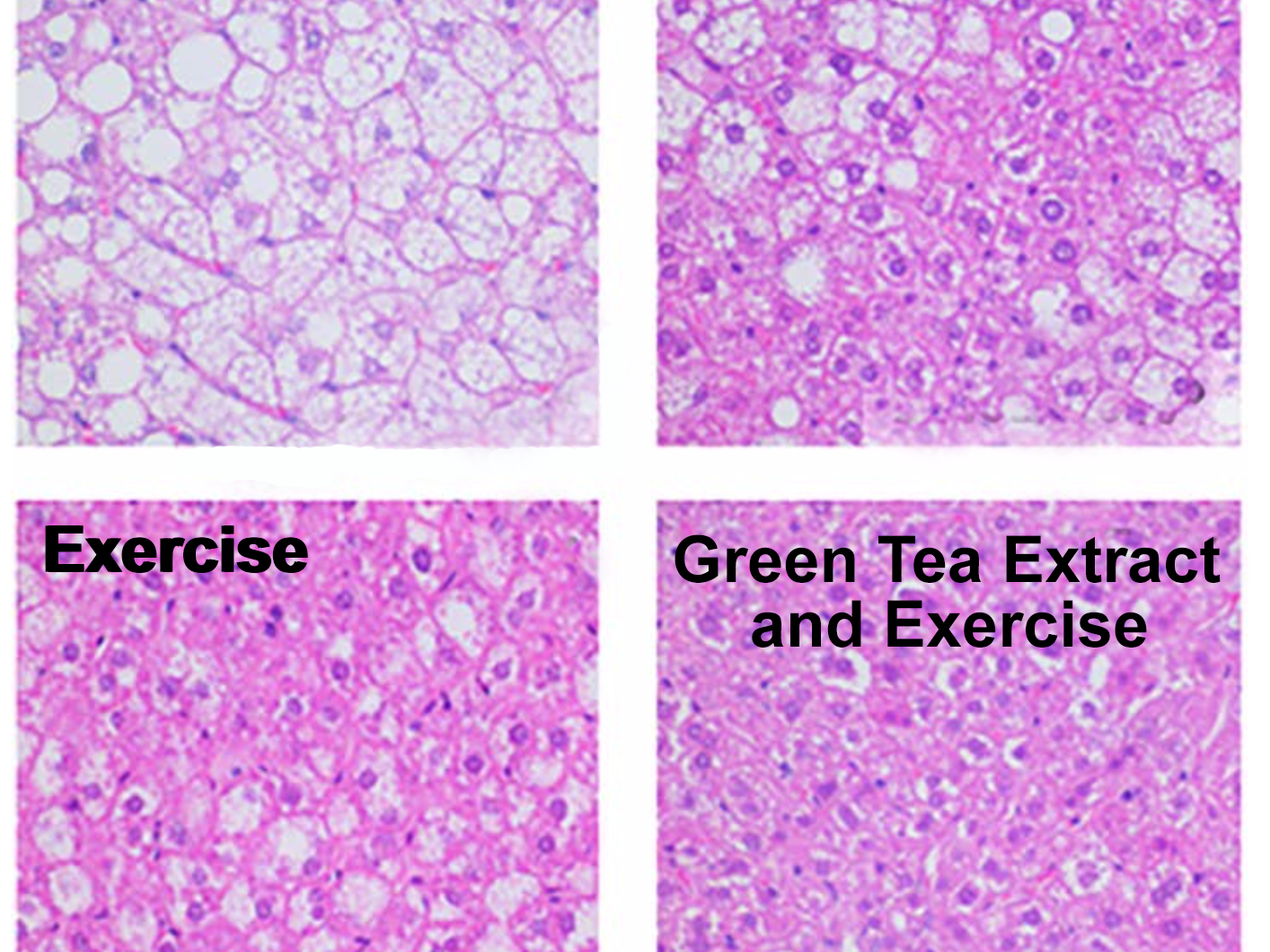
The hepatotoxicity appears to be idiosyncratic rather than dose-dependent, meaning it affects only susceptible individuals. High doses of catechins, particularly epigallocatechin gallate (EGCG) which constitutes 30-50% of green tea extract’s dry weight, are hepatotoxic in animal studies. However, human doses associated with liver injury (typically less than 12 mg/kg daily) generally don’t exceed the estimated direct toxicity threshold of 30-90 mg/kg. This suggests the reaction may be mediated by immune mechanisms or metabolic peculiarities in certain individuals.
Expert Note: Products containing concentrated green tea extract (often labeled as “decaffeinated” or “standardized to 50% EGCG”) pose the highest risk. Whole green tea beverages consumed in normal amounts don’t carry this risk.
OxyELITE Pro’s Deadly Impact: 36 Liver Failures and Hawaii’s Supplement Crisis
In September 2013, Hawaii experienced a shocking outbreak of severe acute hepatitis when seven previously healthy young adults developed jaundice with markedly elevated liver enzymes—all reporting use of OxyELITE Pro as a weight loss and muscle-building agent. Investigators ultimately documented 36 cases of acute liver injury with jaundice linked to this supplement, with one patient dying and two others requiring emergency liver transplantation—a fatality rate of 8%.
How Aegeline Triggered the Liver Injury Epidemic
Chemical analysis revealed the cause was likely the addition of aegeline to OxyELITE Pro in March 2013. Aegeline is the major alkaloid found in the fruit of the bael tree (Aegle marmelos), traditionally used in Ayurvedic medicine. The specific formulation introduced in 2013 may have contained synthetic aegeline with impurities or racemic mixtures that proved hepatotoxic. Clinical features included:
– Mean peak bilirubin: 9.4 mg/dL (range: 2.6 to 41.6)
– Mean ALT: 1,740 U/L (range: 428 to 3,285)
– Mean alkaline phosphatase: 141 U/L (range: 72-277)
Urgent Action: OxyELITE Pro has been removed from the market, but similar products containing aegeline or unlisted ingredients continue to appear under different brand names. Always research ingredients before purchasing weight loss supplements.
Vitamin E’s 40% Liver Cancer Protection: What the Shanghai Study Reveals

While certain supplements dangerously increase liver cancer risk, large-scale epidemiological research reveals vitamin E offers significant protection. Data from the Shanghai Women’s Health Study and Shanghai Men’s Health Study—tracking 132,837 participants over 5-11 years—demonstrated that participants in the highest quartile of dietary vitamin E intake had a 40% reduction in liver cancer risk compared to those in the lowest quartile (hazard ratio 0.60, 95% CI: 0.40-0.89).
Why Vitamin E Works Against Liver Cancer Development
The protective effect extended across all vitamin E subtypes:
– Alpha-tocopherol showed statistically significant risk reduction (P trend=0.04)
– Beta- and gamma-tocopherol demonstrated even stronger protection (P trend=0.01)
– Delta-tocopherol also showed significant benefit (P trend=0.02)
Most compellingly, the protective association persisted among participants who reported no vitamin supplement use at baseline, with those in the highest dietary intake quartile showing 45% lower risk (HR 0.55, 95% CI: 0.35-0.85). This suggests the relationship reflects genuine biological effects rather than confounding by supplement use behavior.
Practical Tip: Get vitamin E from food sources like almonds, sunflower seeds, and spinach rather than high-dose supplements, which may carry other health risks at excessive doses.
Why Multi-Ingredient Supplements Like Herbalife Trigger Liver Damage
The majority (68%) of herbal and dietary supplement-associated liver injury cases involve multi-ingredient nutritional supplements (MINS)—complex formulations containing vitamins, minerals, amino acids, proteins, and botanical extracts. Products like Herbalife, Hydroxycut, Slimquick, and Move Free have all been implicated in liver injury cases, but identifying the specific toxic component proves challenging since these products typically contain 3-20 ingredients with undisclosed concentrations.
The Hidden Danger of “Proprietary Blends”
Manufacturers commonly use the term “proprietary blend” to avoid disclosing specific amounts of each ingredient. This lack of transparency creates serious problems:
– Products may change composition without FDA notification
– Contamination with pharmaceutical agents or toxic botanicals occurs frequently
– Identical products from different batches may contain vastly different ingredient concentrations
Red Flag Alert: If a supplement label lists ingredients but doesn’t specify amounts for each component in a “proprietary blend,” consider it a warning sign of potential risk.
How FDA’s Broken System Fails to Protect You from Toxic Supplements
The Dietary Supplement Health and Education Act of 1994 created a regulatory framework that presumes supplements are safe unless proven otherwise—placing the burden on the FDA to demonstrate harm after products have already injured consumers. Unlike pharmaceuticals that must prove safety and efficacy before market entry, supplements can be sold without pre-market safety testing, with manufacturers only required to submit notification for new dietary ingredients introduced after October 1994.
Critical Gaps in Supplement Regulation
- No mandatory pre-market safety testing: Products enter the market without safety verification
- Inadequate adverse event reporting: Consumers and healthcare providers substantially underreport incidents
- “Proprietary blend” loophole: Allows undisclosed ingredient amounts
- Limited enforcement resources: FDA struggles to monitor 80,000+ supplement products
Proactive Measure: Before buying any supplement, search the FDA’s warning letters database and check for recalls or safety alerts related to the product or manufacturer.
5 Early Warning Signs Your Supplement Is Damaging Your Liver
Supplement-induced liver injury often develops silently before symptoms appear, but recognizing these early warning signs could prevent permanent damage:
- Persistent fatigue that doesn’t improve with rest (often the earliest symptom)
- Dark urine resembling tea or cola (indicating bilirubin buildup)
- Yellowing of the eyes or skin (jaundice), starting with the whites of the eyes
- Unexplained nausea or loss of appetite lasting more than 48 hours
- Abdominal pain in the upper right quadrant where your liver is located
Immediate Action Plan: If you experience any of these symptoms while taking supplements:
– Stop the supplement immediately
– Contact your healthcare provider for liver function tests (ALT, AST, bilirubin, alkaline phosphatase)
– Report the incident to the FDA’s MedWatch program
– Document the supplement’s brand name, lot number, and ingredients
Critical Questions to Ask Before Buying Any Supplement
Protect yourself from dangerous supplements by asking these essential questions before purchase:
- “Does the label list specific amounts for every ingredient?” (Avoid products with “proprietary blends” that hide ingredient concentrations)
- “Has this product or manufacturer received FDA warning letters?” (Check the FDA website)
- “Does this product contain green tea extract, anabolic compounds, or aegeline?” (High-risk ingredients)
- “Is this a single-ingredient product or a complex multi-ingredient formulation?” (Single-ingredient products pose lower risk)
- “What independent testing has verified this product’s contents?” (Look for USP, NSF, or ConsumerLab verification)
Smart Shopping Strategy: Choose supplements that have undergone third-party testing for purity and potency. Organizations like USP, NSF International, and ConsumerLab verify product contents against label claims.
What to Do Immediately If You Suspect Supplement-Induced Liver Damage
If you experience symptoms suggesting liver injury while taking supplements, follow these critical steps:
- Stop taking the supplement immediately—do not wait to see if symptoms improve
- Contact your healthcare provider for blood tests including ALT, AST, bilirubin, and alkaline phosphatase
- Bring the supplement container to your appointment for ingredient verification
- Report the incident to the FDA’s MedWatch program (online or by calling 1-800-FDA-1088)
- Document your timeline of supplement use, symptom onset, and medical evaluations
Expert Recommendation: If you’ve experienced supplement-induced liver injury, avoid all herbal and dietary supplements in the future unless specifically recommended by a healthcare provider who knows your history. When supplements are medically necessary, choose single-ingredient products at the lowest effective dose.
Safer Alternatives to Liver-Damaging Supplements You Can Trust
You don’t have to avoid all supplements to protect your liver—just choose wisely based on scientific evidence:
- For antioxidant protection: Get vitamin E from food sources (almonds, sunflower seeds, spinach) rather than supplements
- For weight management: Focus on evidence-based approaches like portion control and exercise instead of unproven weight loss supplements
- For general wellness: Consider single-ingredient supplements like vitamin D (if deficient) from reputable manufacturers with third-party verification
- For liver support: Milk thistle (silymarin) has evidence for liver protection in some studies, but consult your doctor first
Long-Term Protection Strategy: The most effective way to protect your liver is to address underlying conditions like viral hepatitis, alcohol use, obesity, and diabetes—proven major risk factors for liver cancer that dwarf supplement risks for most people.
Final Note: The complex relationship between dietary supplements and liver cancer reveals both significant risks and potential protections. While certain supplements like anabolic steroids, green tea extract, and multi-ingredient formulations have been linked to dangerous liver injury patterns that may increase cancer risk over time, vitamin E demonstrates a clear protective effect with 40% lower liver cancer risk among high consumers. Protect yourself by avoiding multi-ingredient supplements with undisclosed “proprietary blends,” recognizing early warning signs of liver damage, and choosing single-ingredient products from verified manufacturers. Most importantly, consult your healthcare provider before starting any new supplement—especially if you have existing liver conditions or risk factors for liver disease. Your liver processes everything you ingest, so treat it with the care it deserves by making informed, evidence-based supplement decisions.




