High homocysteine levels silently damage your blood vessels while increasing your risk for heart disease, stroke, and cognitive decline. This amino acid becomes dangerous when your body can’t properly metabolize it due to B vitamin deficiencies or genetic factors. Knowing how to lower homocysteine levels with supplements represents one of the most effective yet overlooked strategies for protecting your cardiovascular and brain health. The good news is that targeted supplementation can often reverse elevated levels within weeks, potentially reducing your risk of serious health complications.
When homocysteine accumulates in your bloodstream, it promotes oxidative stress and impairs your blood vessels’ ability to dilate properly. This process sets the stage for hypertension, atherosclerosis, and increased clot formation—particularly in the delicate vessels of your brain. The most common culprits behind elevated homocysteine are deficiencies in key B vitamins or genetic variations that compromise your body’s ability to process this amino acid efficiently. By understanding which supplements work best and how to use them correctly, you can take control of this critical health marker.
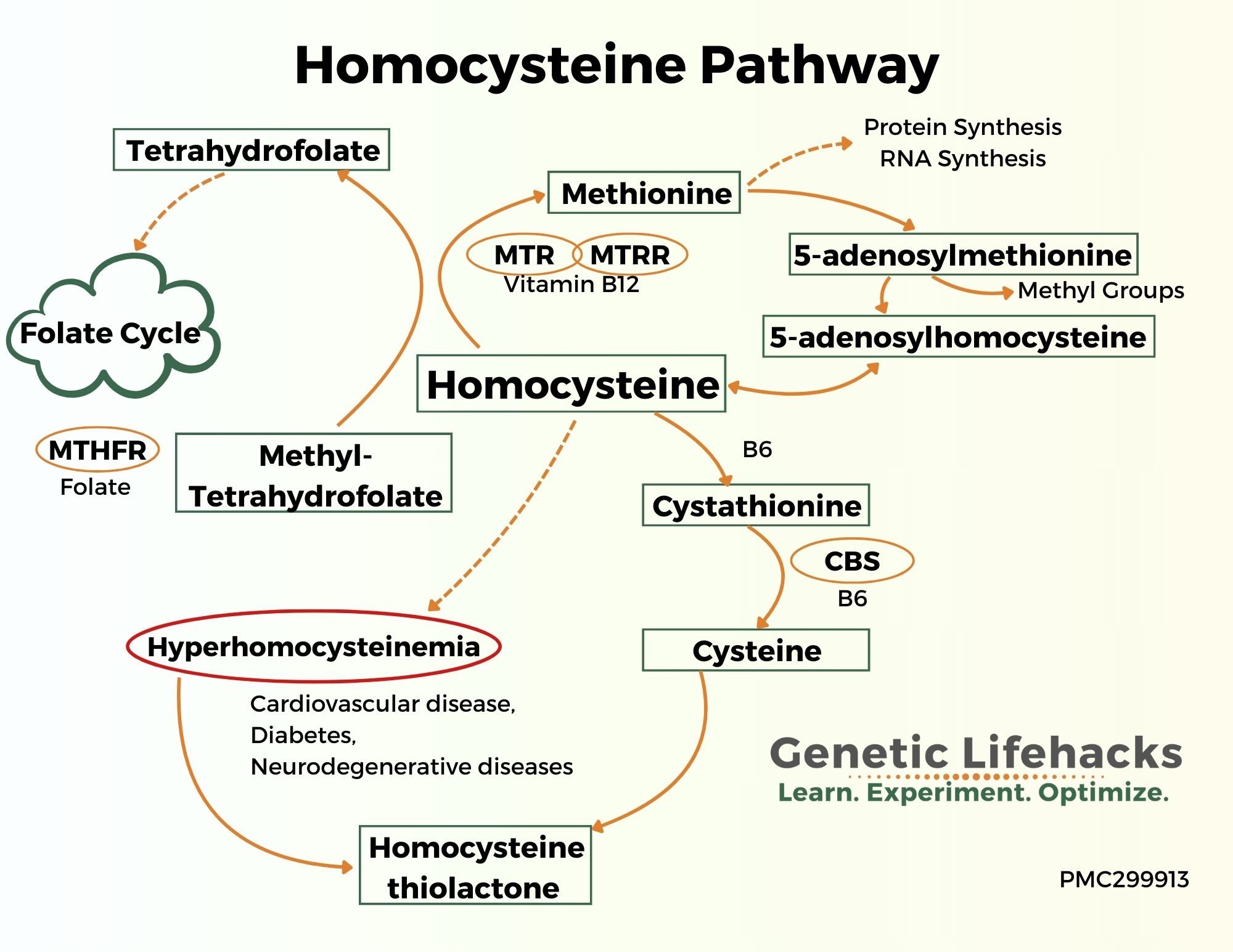
Why Your MTHFR Gene Affects Homocysteine Clearance

Your MTHFR gene provides instructions for creating the enzyme that converts folate into its active form, which is essential for metabolizing homocysteine. Approximately 30% of people carry the C677T genetic variant that reduces this enzyme’s effectiveness, with homozygous individuals (those with two copies) experiencing only about 30% of normal enzyme activity. This genetic difference explains why some people develop high homocysteine despite adequate dietary folate intake.
If you have the MTHFR C677T mutation, you’ll likely need specific forms of supplements to effectively lower homocysteine. Standard folic acid supplements may not work well for you because your body struggles to convert them to the active form. Instead, you’ll benefit more from l-methylfolate (5-methyltetrahydrofolate), which bypasses the compromised enzyme step entirely. This genetic insight explains why personalized supplementation approaches yield dramatically better results than one-size-fits-all solutions.
How to Determine Your Genetic Status
The most reliable way to identify MTHFR variants is through genetic testing, which many direct-to-consumer services now offer. Look for the C677T and A1298C variants, with C677T having the strongest impact on homocysteine metabolism. If genetic testing isn’t accessible, consider your response to standard B vitamin supplements—if homocysteine levels remain elevated despite supplementation, you likely have reduced MTHFR enzyme activity requiring specialized approaches.
Riboflavin: The Overlooked Homocysteine Solution
Riboflavin (vitamin B2) plays a crucial role in homocysteine metabolism that most people completely ignore. For individuals with the MTHFR C677T mutation, riboflavin serves as the essential cofactor FAD that partially compensates for reduced enzyme function. Research shows that as little as 1.6 mg daily of riboflavin can lower systolic blood pressure by 6-13 mm Hg in genetically susceptible individuals—more effectively than some hypertension medications.
This blood pressure reduction carries significant clinical importance since every 2 mm Hg decrease translates to approximately 10% lower stroke risk. The mechanism connects directly to improved homocysteine metabolism, as better processing of this amino acid reduces its damaging effects on cerebral blood vessels. If you have the MTHFR 677TT genotype, riboflavin supplementation represents one of the most powerful yet underutilized interventions available.
Optimal Riboflavin Dosing Strategy
Start with 1.6 mg daily and monitor your homocysteine levels after 8-12 weeks. Some individuals with severe genetic compromise may benefit from higher doses up to 10 mg daily, though most achieve maximum benefit within the lower range. Since riboflavin is water-soluble and excess amounts safely exit through urine, toxicity is extremely rare even at higher doses. Take your riboflavin supplement with breakfast for optimal absorption alongside your other B vitamins.
Folate Form Selection: Why L-Methylfolate Beats Folic Acid
Choosing between folic acid and l-methylfolate makes a dramatic difference in your ability to lower homocysteine levels. Folic acid, the synthetic form found in most supplements and fortified foods, requires multiple conversion steps before your body can use it—steps that are compromised in people with MTHFR variants. This creates a functional folate deficiency even when blood tests show adequate levels.
L-methylfolate (5-methyltetrahydrofolate) bypasses these conversion barriers by providing the active form your body needs immediately. This form also crosses the blood-brain barrier effectively, supporting neurological function while lowering homocysteine. Research shows l-methylfolate produces more consistent homocysteine reduction, especially in individuals with genetic variations affecting folate metabolism.
Supplementing with the Right Folate Form
For optimal results, select supplements containing 400-1000 mcg of l-methylfolate rather than folic acid. Avoid products listing “folic acid” as the folate source, particularly if you have MTHFR variants. Take your folate supplement in the morning with other B vitamins for synergistic effects. Most people see homocysteine reduction within 4-8 weeks of consistent supplementation, though genetic factors may extend this timeline.
Proven B Vitamin Protocol for Homocysteine Reduction
Effective homocysteine management requires all four critical B vitamins working together: riboflavin (B2), pyridoxine (B6), methylcobalamin (B12), and l-methylfolate. Deficiency in any single nutrient can undermine the entire metabolic pathway, causing homocysteine to accumulate despite supplementation with other vitamins.
Your optimal daily protocol should include:
– Riboflavin (B2): 1.6-10 mg (higher for MTHFR 677TT genotype)
– Vitamin B6: 25-100 mg as pyridoxal-5-phosphate
– Vitamin B12: 500-1000 mcg as methylcobalamin
– L-methylfolate: 400-1000 mcg
Take all these supplements together in the morning with food for maximum absorption and synergy. Avoid high-dose standalone B6 supplements exceeding 100 mg daily for extended periods due to potential neuropathy risk.
Timing Your Supplement Intake for Maximum Effect
Consistency matters more than exact timing, but morning dosing aligns best with your body’s natural metabolic rhythms. Take your B vitamin complex with your first meal to enhance absorption and minimize potential digestive upset. If using separate supplements, take them all at the same time to ensure the vitamins work synergistically. Most people notice homocysteine reduction within 4-12 weeks of consistent supplementation.
Interpreting Your Homocysteine Test Results
Understanding what your homocysteine levels mean requires looking beyond standard lab ranges. While many labs consider levels below 15 µmol/L “normal,” research shows that values above 10 µmol/L warrant intervention, and optimal levels likely fall between 5-8 µmol/L. This discrepancy explains why many people with “normal” homocysteine still face elevated cardiovascular risk.
When reviewing your results, pay attention to the trend over time rather than single measurements. A reduction from 14 to 9 µmol/L represents significant progress, even if you haven’t yet reached the optimal range. If your levels remain elevated after 12 weeks of proper supplementation, consider genetic factors, absorption issues, or medication interactions that may require protocol adjustments.
When to Retest After Starting Supplements
Wait at least 8-12 weeks before retesting to allow time for meaningful changes. Testing too soon creates unnecessary expense and frustration when natural fluctuations might mask real progress. Once you achieve target levels, annual monitoring helps maintain your results. If you have H-hypertension (high blood pressure plus elevated homocysteine), consider testing every 6 months until both markers stabilize.
Overcoming Insurance Barriers to Testing
Despite strong evidence linking homocysteine to cardiovascular risk, insurance coverage for testing remains inconsistent. Many providers refuse reimbursement, claiming “lack of clinical utility,” even though elevated homocysteine independently predicts stroke risk and mortality. If your doctor orders the test, be prepared for potential denials and lengthy appeals processes.
Direct-to-consumer testing offers an alternative solution. Several reputable labs now provide homocysteine testing without physician orders for $50-$100—often less than your insurance co-pay would be after denial. These services typically include physician oversight and electronic results you can share with your healthcare provider. While not ideal, this option empowers you to take control of your health metrics when insurance barriers stand in the way.
Special Considerations for High-Risk Groups
Hypertensive patients with elevated homocysteine—what researchers call H-hypertension—represent a population with particularly compelling reasons to address this marker. For every 1 µmol/L increase in homocysteine, hypertensive individuals face 8% higher all-cause mortality risk and 7.15% increased cardiovascular mortality risk. This synergistic relationship means lowering homocysteine may provide greater blood pressure benefits than medication alone for genetically susceptible individuals.
Older adults often need special attention due to age-related declines in B12 absorption. Consider sublingual B12 or higher doses (1000 mcg) to overcome reduced stomach acid production. If you take medications like metformin or proton pump inhibitors, you may need additional B12 supplementation as these drugs interfere with absorption.
Maintaining Your Homocysteine Reduction Long-Term
Achieving optimal homocysteine levels is just the beginning—maintaining them requires ongoing attention. Unlike medications that work only while you take them, B vitamin supplementation creates lasting metabolic improvements but requires consistent intake. Think of it as nutritional maintenance rather than a temporary fix.
Combine your supplementation protocol with a diet rich in natural B vitamins: leafy greens for folate, eggs and dairy for B12, and nuts and seeds for B6. Regular exercise, stress management, and avoiding smoking all support healthy homocysteine metabolism. Schedule annual check-ups to monitor your levels and adjust your protocol as needed based on changing health circumstances.
Key Takeaway: Lowering homocysteine with supplements requires targeted B vitamin support—particularly riboflavin for MTHFR variants, l-methylfolate instead of folic acid, and proper dosing of B6 and B12. This evidence-based approach reduces stroke risk, improves blood pressure control, and supports long-term cardiovascular health. Start with a homocysteine test, implement the right supplement protocol for your genetic profile, and monitor your progress for optimal results.