Approximately 12% of teenagers and a growing number of adults struggle with elevated triglyceride levels, putting them at increased risk for coronary heart disease and, in severe cases, acute pancreatitis. When your fasting blood test shows triglycerides above 150 mg/dL, you’re facing a serious cardiovascular risk factor that operates independently of your cholesterol numbers. While dietary changes and exercise form the foundation of triglyceride management, many people find these lifestyle modifications difficult to maintain consistently—creating legitimate demand for effective supplemental approaches that can provide meaningful support.
Research has identified specific supplements with clinically proven triglyceride-lowering effects, with omega-3 fatty acids emerging as the most extensively studied and reliable option. Understanding exactly how these supplements work, what doses actually produce results, and how to integrate them safely into your health regimen can make the difference between spinning your wheels and achieving measurable improvements in your lipid profile.
This guide cuts through supplement marketing hype to deliver evidence-based strategies for lowering triglycerides with nutritional interventions. You’ll discover precisely which supplements work, how much you actually need to take, and how to combine them with targeted lifestyle changes for maximum impact on your cardiovascular health.
Why High Triglycerides Threaten Your Heart Health
Triglycerides are the primary form of dietary fat and the most abundant lipid stored in your body. When you consume excess calories—particularly from refined carbohydrates and sugar-sweetened beverages—your liver converts these into triglycerides for storage in fat tissue. This metabolic process explains why modern diets heavy in processed foods directly fuel elevated triglyceride levels that show up on your blood panel.
Fasting triglyceride levels above 150 mg/dL indicate hypertriglyceridemia, which creates multiple cardiovascular dangers. High triglycerides often accompany low HDL (“good”) cholesterol, small dense LDL particles, and insulin resistance—forming a dangerous metabolic combination that accelerates atherosclerotic plaque development. What many people don’t realize is that triglycerides represent an independent risk factor; even with normal cholesterol readings, elevated triglycerides still increase your heart disease risk.
The real challenge most people face is that lifestyle changes alone often yield inconsistent results. Dietary modifications require sustained effort, exercise demands consistent time commitment, and weight loss proves difficult to maintain long-term. This reality makes evidence-based supplementation a valuable complementary strategy—not a replacement for healthy habits, but a practical support system that bridges the gap when lifestyle changes fall short.
How Omega-3 Fatty Acids Target Triglyceride Production
The Multi-Pronged Mechanism That Lowers Blood Triglycerides
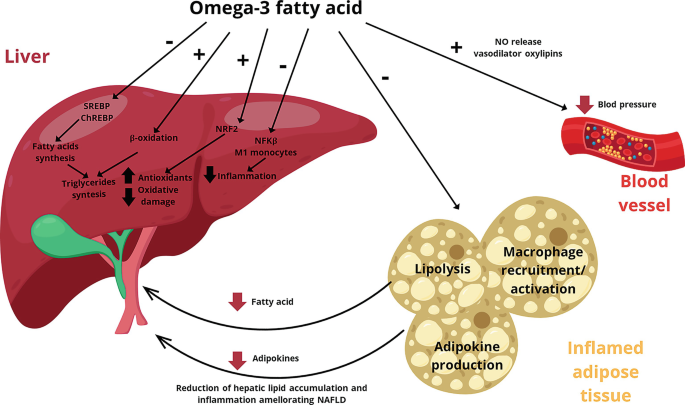
EPA and DHA—the long-chain omega-3 fatty acids found in fish oil—lower triglycerides through three distinct biological pathways that work simultaneously. These essential fats reduce triglyceride synthesis in your liver, increase breakdown of existing triglycerides, and accelerate clearance from your bloodstream. This triple-action approach explains why omega-3s outperform single-mechanism interventions for triglyceride management.
Unlike medications that target only one aspect of lipid metabolism, omega-3s provide additional cardiovascular benefits beyond triglyceride reduction. They serve as structural components of every cell membrane, influence inflammation pathways, and support endothelial function—addressing multiple aspects of cardiovascular health with a single intervention.
Proven Dosing That Delivers Measurable Results

Research shows a clear dose-response relationship: higher omega-3 doses produce greater triglyceride reductions. For clinically meaningful results, you need 2-4 grams daily of combined EPA and DHA—not total fish oil content. This distinction is critical because a standard 1,000 mg fish oil capsule typically contains only 300-400 mg of actual EPA and DHA.
Pharmaceutical-grade options like Lovaza concentrate these active components more efficiently, with each 1,000 mg capsule delivering 840 mg of omega-3s (465 mg EPA and 375 mg DHA). This means therapeutic dosing requires either:
– 5-10 standard fish oil capsules daily, or
– 3-4 pharmaceutical-grade capsules
Important: Always consult your physician before starting high-dose omega-3 supplementation, especially if you take blood thinners or have significant hypertriglyceridemia (above 300 mg/dL).
Niacin: The Powerful but Tricky Alternative
How High-Dose Niacin Affects Multiple Lipid Markers
Niacin (vitamin B3) works differently than omega-3s by targeting multiple lipid parameters simultaneously. At pharmacological doses (above 1,000 mg daily), niacin lowers triglycerides, increases HDL cholesterol, and reduces LDL cholesterol. This broad-spectrum effect makes it valuable for people with complex lipid abnormalities, but requires medical supervision due to significant side effects.
The exact mechanism involves activation of specific cellular receptors that regulate lipid metabolism. Unlike omega-3s which primarily affect triglyceride processing, niacin influences the production and clearance of multiple lipoprotein particles—explaining its wider impact on your overall lipid profile.
Managing Niacin’s Notorious Side Effects
The most common and bothersome side effect of high-dose niacin is flushing—intense warmth, redness, and itching typically affecting the face and upper body. This reaction, while harmless, causes many people to discontinue treatment. Use these evidence-based strategies to improve tolerability:
- Take with meals to slow absorption and reduce flushing intensity
- Use aspirin (81-325 mg) 30 minutes before niacin to block prostaglandin release
- Choose extended-release formulations that release niacin more gradually
- Start low and go slow—begin with 250-500 mg daily and gradually increase
Critical warning: Never attempt high-dose niacin therapy without medical supervision. Liver function requires regular monitoring, and niacin can worsen blood sugar control in people with diabetes.
Maximizing Supplement Effectiveness with Strategic Lifestyle Changes
The Essential Dietary Modifications That Boost Supplement Results
Supplements work best when combined with specific dietary changes that address the root causes of high triglycerides. Focus on these evidence-based dietary strategies that directly impact triglyceride production:
- Eliminate sugar-sweetened beverages—a single 12-ounce soda provides enough fructose to significantly increase liver triglyceride production
- Reduce refined carbohydrates—white bread, pastries, and processed snacks convert directly to triglycerides
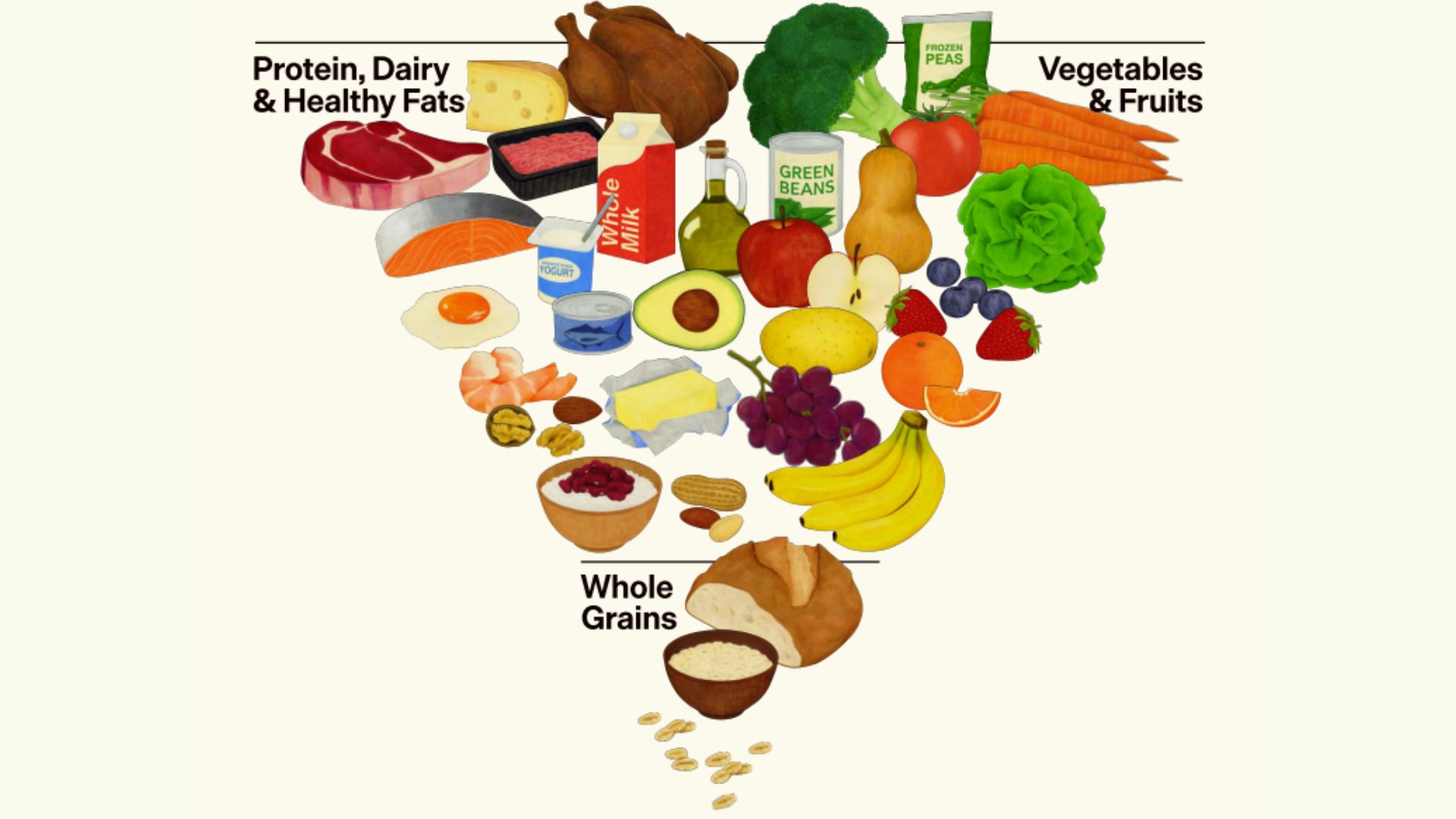
- Increase omega-3 rich foods—consume at least two 3.5-ounce servings of fatty fish weekly to complement supplementation
- Boost fiber intake—aim for 25-30 grams daily from vegetables, fruits, and whole grains to improve lipid metabolism
Pro tip: Track your carbohydrate intake using a food diary app for one week. If more than 50% of your calories come from carbs (especially refined sources), prioritize reducing this percentage to see faster triglyceride improvements.
Creating Your Personalized Supplement Protocol
Follow this step-by-step approach to implement an effective supplement strategy:
- Get baseline testing: Request a fasting lipid panel before starting supplements
- Start with omega-3s: Begin with 2 grams of combined EPA/DHA daily for mild elevation (150-200 mg/dL)
- Adjust based on severity: Increase to 3-4 grams daily if triglycerides exceed 200 mg/dL
- Re-test after 8-12 weeks: Monitor response before making dose adjustments
- Consider niacin only if needed: Add under medical supervision if omega-3s alone don’t produce sufficient reduction
Common mistake: Taking insufficient doses. Many people use 1 gram of fish oil daily (providing only 300 mg EPA/DHA) and wonder why they see no results. Therapeutic dosing requires significantly higher amounts.
When to Seek Medical Guidance for Supplement Use
Red Flags Requiring Immediate Physician Consultation
While omega-3 supplements are generally safe for most adults, certain situations demand professional medical involvement:
- Triglycerides above 500 mg/dL: This severe elevation requires medical supervision due to pancreatitis risk
- Taking blood thinners: Omega-3s have mild anticoagulant effects that may interact with medications
- Upcoming surgery: Discontinue high-dose omega-3s 7-10 days before procedures
- Liver disease: Requires careful monitoring with both omega-3 and niacin therapy
- Diabetes: Niacin can worsen blood sugar control and requires close management
Critical point: Supplements are not replacements for prescribed medications in cases of severe hypertriglyceridemia. Work with your physician to determine whether supplements alone or in combination with medications best addresses your specific situation.
Tracking Your Progress and Adjusting Your Approach
The Monitoring Protocol That Ensures Results
Effective triglyceride management requires systematic tracking to assess what’s working. Follow this evidence-based monitoring schedule:
- Baseline test: Fasting lipid panel before starting supplements
- 8-12 week follow-up: First assessment of supplement effectiveness
- 3-6 month retest: Confirm sustained improvement and adjust as needed
- Annual testing: Ongoing monitoring even after reaching target levels
When reviewing your results, look beyond just triglyceride numbers. Track improvements in related markers like HDL cholesterol, inflammatory markers (C-reactive protein), and insulin sensitivity—these provide a more complete picture of your cardiovascular risk reduction.
Pro tip: If triglycerides haven’t decreased by at least 20% after 12 weeks of proper dosing, consult your physician about adding niacin therapy or other interventions. Don’t continue ineffective protocols out of hope that “more time” will produce results.
The Most Effective Supplement Strategy for Lowering Triglycerides
For most people seeking to lower triglyceride levels with supplements, omega-3 fatty acids at 2-4 grams of combined EPA/DHA daily represent the safest and most effective starting point. This dose range produces clinically meaningful 25-30% reductions in triglyceride levels for most individuals, with minimal side effects when implemented properly.
While niacin offers additional benefits for complex lipid profiles, its side effect profile makes it a secondary option that requires medical supervision. The most successful approach combines appropriate supplementation with targeted dietary changes—specifically reducing refined carbohydrates and added sugars while increasing omega-3 rich foods.
Remember: Supplements support but don’t replace healthy lifestyle habits. The combination of evidence-based supplementation with strategic dietary modifications delivers the most reliable, sustainable results for lowering triglycerides and improving your overall cardiovascular health profile. Work with your healthcare provider to develop a personalized plan that addresses your specific lipid profile and health circumstances for optimal results.




