Magnesium powers over 300 enzymatic reactions in your body, yet nearly half of Americans fail to get enough through diet alone. This essential mineral regulates everything from muscle contractions and nerve function to blood sugar control and blood pressure regulation. When your magnesium levels dip below optimal ranges, you might experience muscle cramps, fatigue, irregular heartbeat, or even increased risk for chronic conditions like diabetes and cardiovascular disease. These evidence-based magnesium supplementation guidelines will help you identify if you need supplemental magnesium, determine the right dosage for your specific health needs, and select the most effective form to maximize absorption while avoiding potential side effects.
Many people mistakenly believe that taking any magnesium supplement will solve their problems, but improper dosing or choosing the wrong form can lead to wasted money or uncomfortable digestive issues. Following these magnesium supplementation guidelines ensures you’re addressing your body’s actual needs without risking adverse effects from excessive intake. Whether you’re managing specific health concerns or simply aiming to optimize your wellness routine, understanding how much magnesium you need and which form works best for your physiology makes all the difference in achieving tangible health benefits.
Why Your Body Can’t Function Without Adequate Magnesium
Magnesium serves as the critical spark plug for your cellular engine, activating more than 300 enzyme systems that drive essential bodily functions. Your body stores approximately 25 grams of this mineral, with 60% embedded in your bones and the rest distributed primarily in muscle tissue and soft organs. What many people don’t realize is that less than 1% of your total magnesium circulates in your blood—this tiny fraction is tightly regulated between 0.75 to 0.95 millimoles per liter, making blood tests an unreliable indicator of your overall magnesium status.
The Energy Production Connection You Need to Understand
Your cells convert food into usable energy through processes that absolutely require magnesium. Without sufficient magnesium, your mitochondria struggle to produce ATP—the energy currency of your cells—because magnesium forms a complex with ATP (MgATP) that’s necessary for energy transfer. This explains why magnesium deficiency often manifests as persistent fatigue, muscle weakness, and exercise intolerance. When your magnesium levels drop, your body literally runs out of fuel faster, leaving you feeling drained even after adequate rest.
How Magnesium Regulates Critical Body Systems
Beyond energy production, magnesium acts as the body’s natural calcium channel blocker, controlling the flow of calcium across cell membranes. This regulatory function explains magnesium’s profound impact on heart rhythm, muscle contractions, and nerve signaling. When magnesium levels fall too low, calcium floods into cells unchecked, triggering muscle spasms, abnormal heart rhythms, and nerve excitability that can cause tingling or numbness. Magnesium also serves as the essential cofactor for parathyroid hormone—without adequate magnesium, your body can’t properly regulate calcium levels, leading to a cascade of metabolic disturbances.
Daily Magnesium Requirements That Actually Work for You
The National Academies of Sciences, Engineering, and Medicine established precise magnesium requirements based on age, sex, and life stage—these aren’t arbitrary numbers but reflect your body’s actual physiological needs. Men aged 19-30 require 400 mg daily, while women in the same age bracket need 310 mg. After age 31, men’s requirements increase to 420 mg while women need 320 mg. These numbers represent total intake from all sources—food, beverages, supplements, and medications—so you’ll need to assess your current dietary intake before adding supplements.
Critical Age-Specific Requirements You Must Know
Teenage boys (14-18 years) have the highest daily requirement at 410 mg, while girls their age need 360 mg. During pregnancy, adolescent females require 400 mg daily, whereas adult pregnant women need 350-360 mg depending on age. Breastfeeding women should maintain intake at 310-360 mg daily. Children’s requirements vary significantly by age group: 80 mg for ages 1-3, 130 mg for ages 4-8, and 240 mg for ages 9-13. Infants need substantially less—30 mg for the first six months and 75 mg from 7-12 months.
Why Most People Fall Short of These Targets
Despite these clear requirements, dietary surveys reveal alarming gaps in magnesium intake. Men over 70 and teenagers of both sexes are most likely to consume less than recommended amounts. The typical Western diet—high in processed foods and low in magnesium-rich whole foods—contributes significantly to this widespread shortfall. When you factor in modern farming practices that have depleted soil magnesium levels, even “healthy” diets often fall short of optimal magnesium intake.
How to Identify Hidden Magnesium Deficiency Symptoms
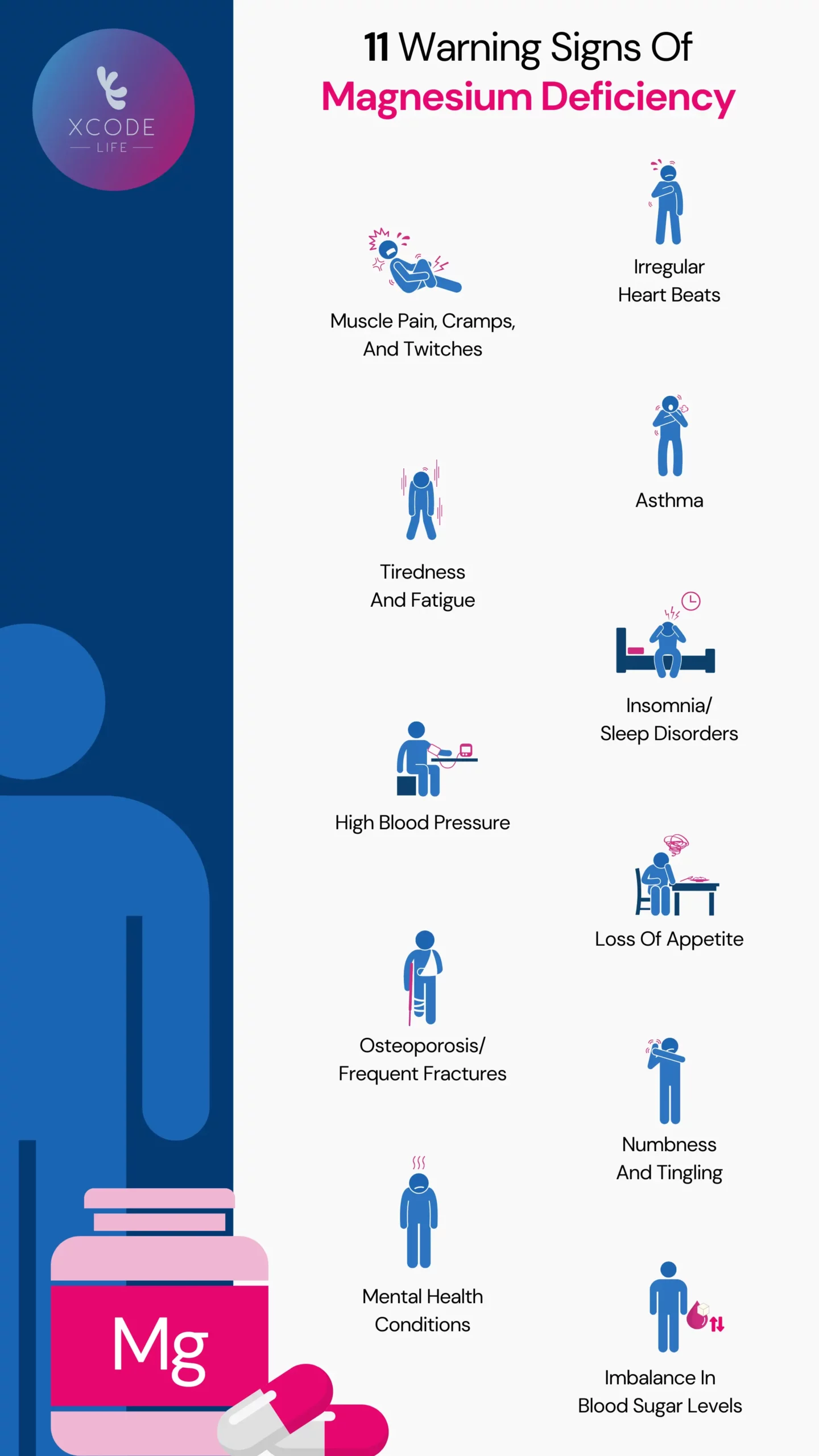
Magnesium deficiency often masquerades as other health issues, making it crucial to recognize these subtle warning signs before they escalate into serious complications. Early deficiency typically presents with nonspecific symptoms like persistent fatigue, muscle cramps (especially at night), and loss of appetite. As depletion worsens, you might experience nausea, vomiting, personality changes, or abnormal heart rhythms. Severe deficiency can trigger numbness, tingling, seizures, and life-threatening cardiac arrhythmias.
The Surprising Calcium-Magnesium Connection
One of the most overlooked magnesium deficiency indicators involves calcium regulation. When your magnesium levels drop too low, your body develops resistance to parathyroid hormone—even with normal calcium intake, your blood calcium levels decrease. This explains why some people continue experiencing muscle spasms and cramps despite adequate calcium supplementation. If you’ve been taking calcium supplements without relief from these symptoms, magnesium deficiency might be the missing piece.
High-Risk Groups That Need Immediate Attention
Certain populations face dramatically increased magnesium deficiency risk and should prioritize testing and supplementation. People with gastrointestinal disorders like Crohn’s disease or celiac face malabsorption issues. Chronic alcoholics often develop deficiency due to poor intake and increased urinary excretion. Older adults experience declining absorption and increased excretion. If you take diuretics for hypertension, you’re losing magnesium through urine at an accelerated rate. Anyone with these risk factors should consult their healthcare provider about magnesium testing before symptoms appear.
Choosing the Right Magnesium Supplement Form for Your Needs

Not all magnesium supplements deliver equal benefits—selecting the appropriate form makes the difference between experiencing dramatic improvements and wasting money on ineffective products. Magnesium citrate offers superior absorption (up to 25% higher than oxide forms) and works exceptionally well for general supplementation. If you struggle with digestive upset from other forms, magnesium glycinate provides excellent absorption with minimal gastrointestinal effects due to its binding with the amino acid glycine.
The Bioavailability Breakdown You Need
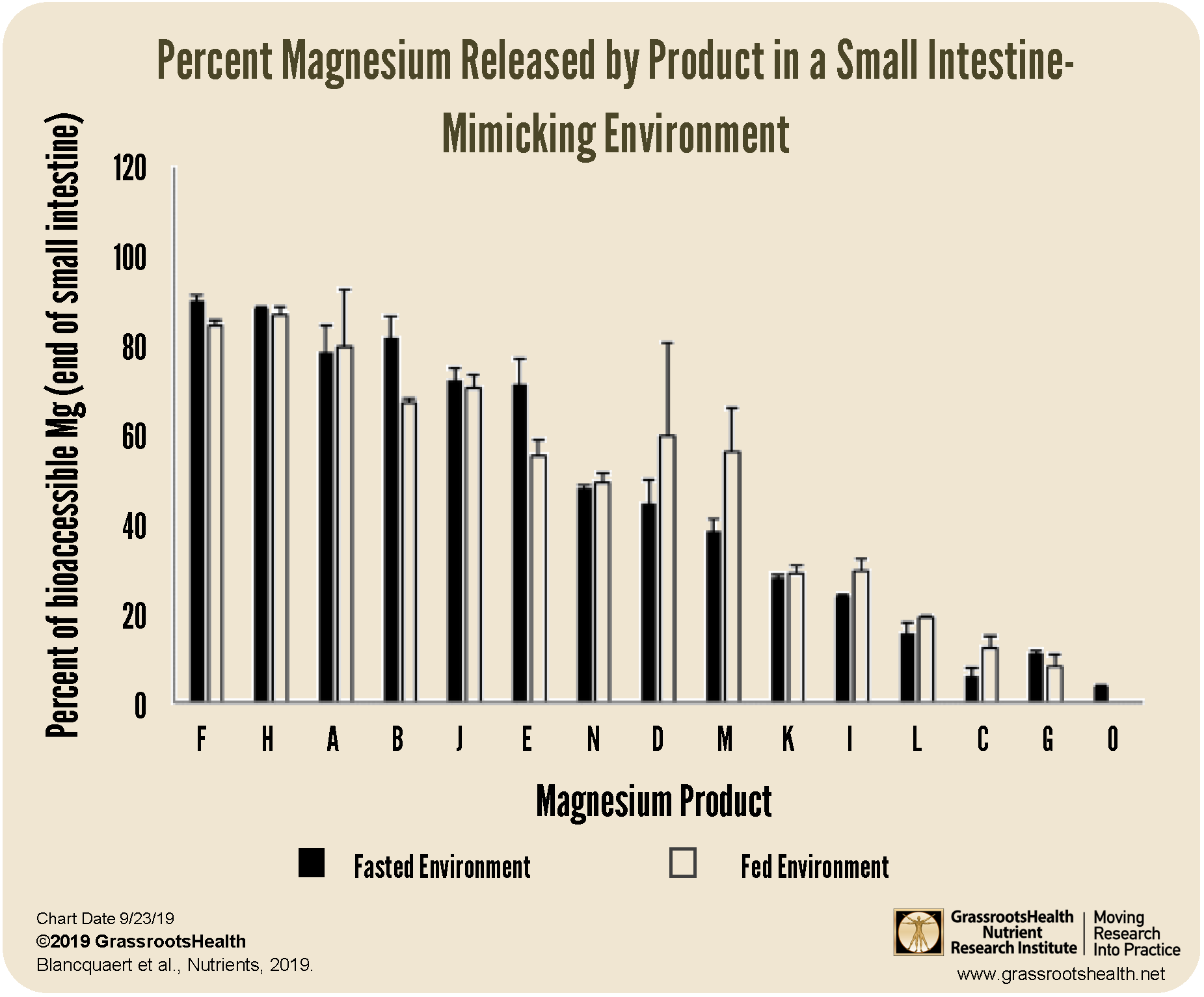
When comparing supplements, focus on elemental magnesium content—the actual amount of usable magnesium—not the total compound weight. Magnesium oxide contains 60% elemental magnesium but has poor absorption (only about 4%), making it suitable primarily for constipation relief. Magnesium chloride delivers 12% elemental magnesium with good absorption, while magnesium lactate offers 11.2% elemental magnesium with high bioavailability. For cognitive benefits, magnesium L-threonate crosses the blood-brain barrier more effectively than other forms, though research is still emerging on its long-term benefits.
Timing and Dosage Strategies for Maximum Effect
Split your daily magnesium dose into two or three smaller servings taken with meals to enhance absorption and minimize digestive side effects. Start with 100-150 mg of elemental magnesium twice daily, then gradually increase to your target dose over two weeks. Never exceed 350 mg of supplemental magnesium daily unless under medical supervision—this upper limit prevents diarrhea and other adverse effects. Take magnesium supplements at least two hours before or after antibiotics, bisphosphonates, or medications that reduce stomach acid, as these can interfere with absorption.
Critical Safety Guidelines for Supplementing Without Side Effects
Exceeding safe magnesium intake levels triggers uncomfortable—and potentially dangerous—side effects that many supplement users mistakenly attribute to other causes. Doses above 350 mg of supplemental magnesium daily commonly cause diarrhea, nausea, and abdominal cramping as unabsorbed magnesium draws water into the intestines. Extremely high doses can lead to irregular heartbeat, muscle weakness, and in severe cases, cardiac arrest—particularly dangerous for people with kidney impairment who can’t efficiently excrete excess magnesium.
Essential Drug Interaction Warnings You Must Know
Magnesium supplements significantly reduce absorption of bisphosphonates (osteoporosis medications) when taken within two hours. Certain antibiotics—including tetracyclines and quinolones—bind to magnesium, rendering both the antibiotic and magnesium ineffective. Proton pump inhibitors for acid reflux decrease magnesium absorption over time, creating a dangerous cycle where the medication causes deficiency that then requires supplementation. Always consult your pharmacist about potential interactions with your current medications before starting magnesium supplementation.
Special Population Considerations for Safe Use
Pregnant women should maintain magnesium intake between 350-400 mg daily but avoid exceeding upper limits without medical supervision. Older adults often need supplementation due to decreased absorption but require lower doses to prevent accumulation. People with kidney disease must work closely with their nephrologist to determine safe magnesium levels, as impaired kidney function drastically reduces excretion capacity. If you have a history of kidney stones, discuss magnesium supplementation with your urologist, as certain forms may affect stone formation.
Creating Your Personalized Magnesium Supplementation Plan
Start by tracking your current dietary magnesium intake for three days using a nutrition app—most adults get only 200-300 mg from food, leaving a significant gap to fill. Calculate your deficit by subtracting your average intake from the recommended daily amount for your age and sex. Begin supplementation with half your calculated deficit dose for the first week, then increase to the full amount if no digestive issues occur. For example, if you need 120 mg additional magnesium daily, start with 60 mg for seven days before increasing to 120 mg.
Monitoring Your Progress and Adjusting as Needed
Track symptom changes in a journal for the first 60 days of supplementation—note improvements in sleep quality, muscle cramps, energy levels, and stress management. If you experience loose stools, reduce your dose by 50 mg and maintain that level for two weeks before attempting to increase again. After three months of consistent supplementation, consider consulting your healthcare provider about a serum magnesium test, though remember this only reflects 1% of your total body stores and may appear normal even with cellular deficiency.
Long-Term Maintenance Strategies for Sustained Benefits
Once you’ve achieved optimal magnesium status, focus on maintaining levels through dietary sources supplemented with a lower maintenance dose. Incorporate magnesium-rich foods like spinach, almonds, black beans, and avocado into daily meals. Continue taking 100-200 mg of supplemental magnesium daily, preferably in the evening when it can support relaxation and sleep quality. Every six months, reassess your dietary intake and symptoms to determine if dosage adjustments are needed based on lifestyle changes or health status shifts. Remember that consistent, moderate supplementation yields better long-term results than sporadic high-dose approaches.